INTRODUCTION
As per WHO – Noncommunicable diseases (NCDs), also known as chronic diseases, tend to be of long duration and are the result of a combination of genetic, physiological, environmental and behavioural factors.
The main types of NCD are cardiovascular diseases (such as heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma) and diabetes.
NCDs disproportionately affect people in low- and middle-income countries, where more than three quarters of global NCD deaths (31.4 million) occur.
RISK FACTORS FOR NON-COMMUNICABLE DISEASES
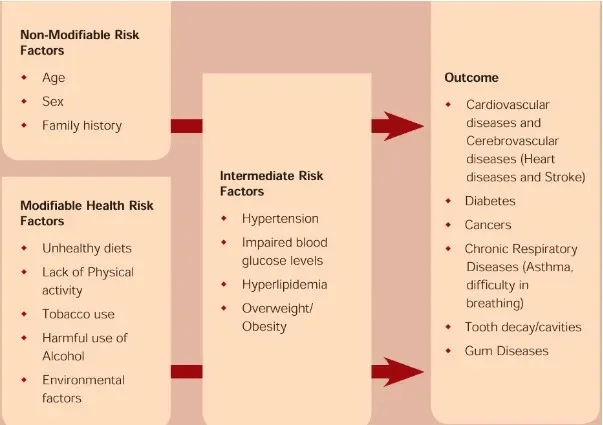
A risk factor is any condition or behavior that increases the likelihood of developing a disease, injury, or other health issue. Risk factors contribute to the onset of non-communicable diseases, and having multiple risk factors heightens the probability of acquiring a specific disease.
ISSUES
The escalation of non-communicable diseases in India can be linked to a mix of lifestyle, environmental, and socio-economic influences. Key factors contributing to this trend include:
- Urbanization and Sedentary Lifestyles: The rapid expansion of urban areas has led to more sedentary occupations, decreased physical activity, and greater reliance on motorized transport.
- Dietary Changes: There is an increasing preference for processed and high-calorie foods over traditional diets, resulting in obesity and associated health issues.
- Air Pollution: Elevated levels of air pollution, particularly in urban areas, are linked to respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD).
- Tobacco and Alcohol Use: Despite various awareness initiatives, tobacco and alcohol use remains widespread, raising the risk of cancers, cardiovascular diseases, and liver disorders.
- Stress and Mental Health Issues: Modern life pressures, including work-related stress and challenges of urban living, have led to a rise in mental health disorders, which are often associated with other NCDs.
- Limited Preventive Healthcare Access: Many individuals lack regular health check-ups and early diagnostic services, resulting in late detection and management of NCDs.
IMPLICATIONS
- Intergenerational Impact: NCDs can affect not only the individual but also future generations. For example, conditions like gestational diabetes can elevate the risk of both the mother and child developing diabetes later, perpetuating a cycle of disease.
- Shift in Healthcare Priorities: As NCDs become more common, healthcare focus may shift from infectious diseases to chronic disease management, potentially neglecting other crucial health areas like maternal and child health and infectious disease control.
- Rural Healthcare Challenges: The rise of NCDs in rural areas, where healthcare infrastructure is often lacking, presents unique challenges. Limited access to specialized care and diagnostic facilities exacerbates the impact, leading to higher mortality and morbidity.
- Cultural and Behavioral Shifts: The increase in NCDs often brings about changes in social norms and behaviors, such as greater emphasis on fitness. However, this may create disparities where only those with resources can fully engage in preventive measures like gym memberships or healthy diets.
- Impact on National Security: In countries with high NCD prevalence, the health of military personnel and the broader workforce can be affected, potentially impacting national security and preparedness. Chronic diseases among young adults can reduce the pool of fit individuals available for military service or physically demanding jobs.
INITIATIVES
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS): This program focuses on preventing and managing major NCDs through early diagnosis, treatment, and awareness campaigns.
- National Health Mission (NHM): The NHM integrates NCD prevention and control into a broader health strategy, providing funding for healthcare infrastructure, health education, and community outreach.
- Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PM-JAY): This health insurance scheme offers coverage for secondary and tertiary care, including treatment for NCDs, aiming to reduce out-of-pocket expenses.
- National Tobacco Control Programme (NTCP): This initiative aims to reduce tobacco use through public awareness campaigns, stricter regulations on tobacco advertising, and smoking cessation programs.
- National Alcoholism and Drug Dependence Programme: This program addresses alcohol and drug abuse, which are risk factors for NCDs, through rehabilitation, counseling, and awareness efforts.
- Health and Wellness Centres (HWCs): Under Ayushman Bharat, HWCs provide comprehensive primary health care services, including NCD screening and management.
- National Cancer Grid: This initiative establishes a network of cancer centers to improve access to quality care, promote research, and develop standard treatment protocols.
- National Institute for Research in Reproductive and Child Health (NIRRCH): This institute conducts research on reproductive health and the impact of NCDs on maternal and child health.
INNOVATION
- AI-driven Personalized Health Platforms: Utilize wearable data, genetics, and lifestyle information to provide customized health advice, aiding in the early detection and prevention of NCDs like diabetes and heart disease.
- Community-Based Digital Health Ambassadors: Train local individuals to use apps for tracking NCD risks and providing health education, enhancing access to health information in communities.
- Smart Nutritional Labeling Systems: Employ QR codes on food packaging to offer personalized dietary advice, encouraging healthier food choices based on individual health data.
- Remote Chronic Disease Monitoring: Implement telehealth solutions to allow patients to monitor and manage chronic conditions from home, reducing the need for frequent hospital visits and improving long-term outcomes.
- Gamification of Healthy Lifestyle Choices: Develop apps and platforms that use gamification to encourage physical activity, healthy eating, and regular health check-ups, making healthy habits more engaging.
- Mobile Health Clinics: Deploy mobile health units to underserved areas to provide screenings, education, and treatment for NCDs, improving care access in remote locations.
- Genetic Screening and Counseling Programs: Provide accessible genetic screening and counseling to identify individuals at high risk for NCDs, enabling early interventions and personalized prevention strategies.
- Social Support Networks for Chronic Disease Management: Create online platforms where NCD patients can connect, share experiences, and receive emotional support, helping them manage their conditions and reduce isolation.
CONCLUSION
Non-communicable diseases (NCDs) such as heart disease, cancer, diabetes, and chronic respiratory conditions are major global health issues, driven by poor diet, inactivity, tobacco use, and alcohol consumption. Addressing NCDs requires more than traditional healthcare; it necessitates innovative strategies focused on prevention and early intervention. Technological advancements like AI-driven health platforms, community health ambassadors, and smart nutritional labeling empower individuals to make healthier choices. Remote monitoring and gamified health apps engage people in proactive health management. Mobile clinics and genetic screening programs can enhance care in underserved areas, while social support networks offer emotional resilience for chronic condition management. Effective NCD management requires scalable, innovative solutions that emphasize prevention, early detection, and ongoing support to improve global health outcomes.
KEY FACTS
- Noncommunicable diseases (NCDs) are responsible for 41 million deaths annually, representing 74% of all global deaths.
- Each year, 17 million people die from NCDs before the age of 70, with 86% of these premature deaths occurring in low- and middle-income countries.
- Low- and middle-income countries account for 77% of all NCD deaths.
- Cardiovascular diseases lead NCD deaths, with 17.9 million annually, followed by cancers (9.3 million), chronic respiratory diseases (4.1 million), and diabetes (2.0 million, including deaths from kidney disease due to diabetes).
- These four disease categories account for over 80% of all premature NCD deaths.
- Tobacco use, physical inactivity, excessive alcohol consumption, unhealthy diets, and air pollution all contribute to increased risk of NCD mortality.
- Key responses to NCDs include detection, screening, treatment, and palliative care.
